Radical Tenderness —and Before Naloxone, Bread
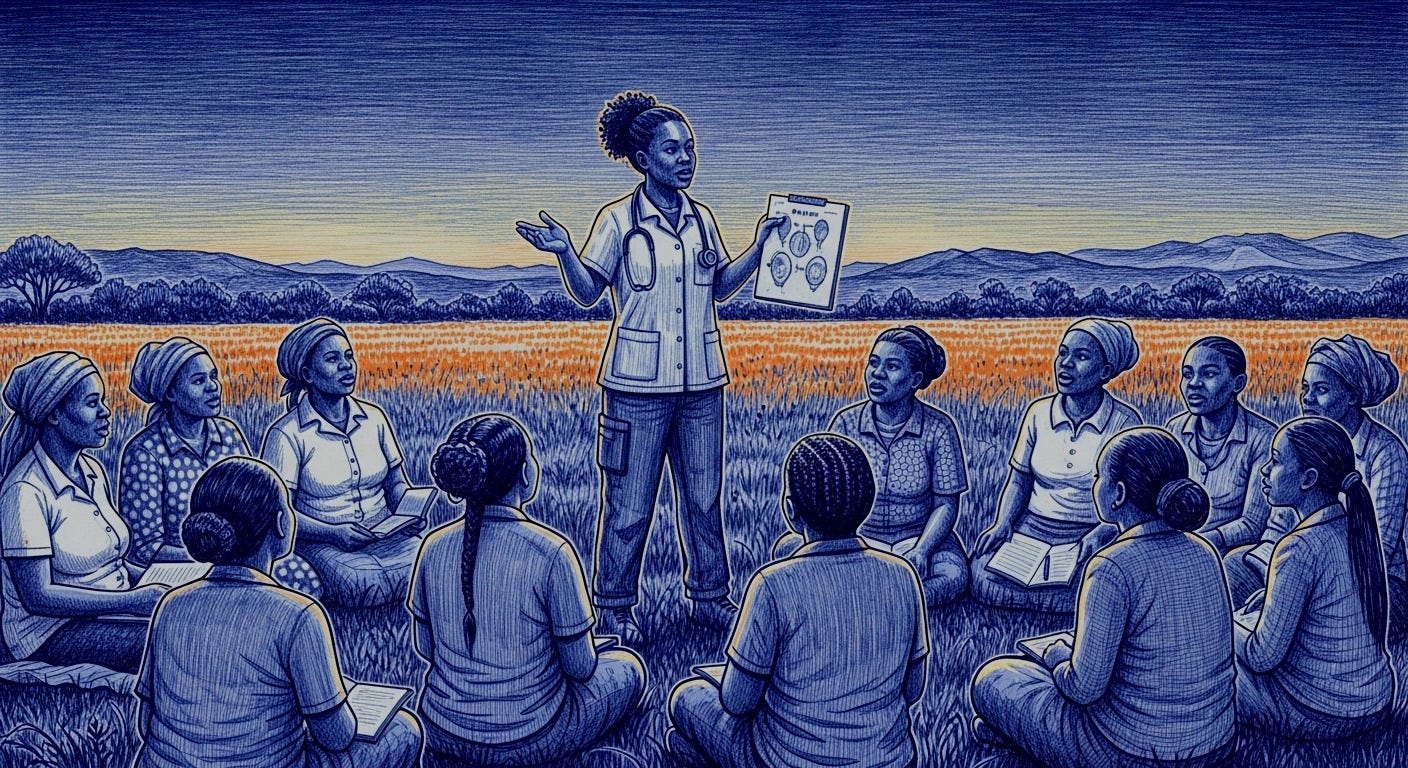
What an African seminar left us with: when services ignore gender and community, they fail; without listening, data is useless; tenderness is a methodology, too.
Julie MacDonnell, Caron Mathews, Kalvanya “Kal” Padayachee, Dimakatso “Dee” Nonyane, Aura Roig, Daniela Sefora Goeieman, and Colleen Daniels open a window — and a mirror — onto an uncomfortable, urgent promise: to design gender-informed harm reduction in Africa. What followed was a living map of community practices and difficult questions, shot through with a simple, fierce idea: tend first to the basics—bread, shelter, safety —in order to rewrite harm reduction.
The Rectangle of Light
When you press play, the screen works as both a window and a mirror. In the background, a lake as wide as a held breath. Mountains edged with snow and, to the right, a tree keeping watch at the border.
It could be a real landscape, or a photograph placed there to remind us that horizons still exist beyond the pixels.
In the foreground, centered, a woman smiles calmly. The webcam’s flat light polishes her cheekbones and leaves glints on her forehead. Her black hair is loose, parted in the middle, falling in symmetry. In one ear, a tiny earpiece: the other voice enters on a thread.
Over a dark sweater, a beaded pectoral bursts into multicolored zigzags, as if the body’s geography were also a map of possible routes.
Red, blue, green, yellow, white: it keeps its own pulse, an intimate cartography made of patience, listening, and hands. It needs no explanation: it claims the frame, lifts the mood, and defies the gray of any meeting room. If the background promises distance, that necklace—together with the smile and the gaze—restores proximity.
The smile says “I’m here,” even if the body is elsewhere. A little over a year ago, Julie MacDonnell—a harm-reduction and human-rights consultant in Cape Town- opened an online seminar on gender-focused harm reduction in Africa. Against the gridded constraints of the video call—that bureaucratic stamp of distance—her look certifies that there is conversation. It wasn’t just another event; it was an effort to name what the system usually leaves outside the frame.
Participants included Caron Mathews (first-person testimony), Kalvanya Padayachee (African Women in Harm Reduction Group, AWHRG), Dimakatso “Dee” Nonyane (COSUP’s community model), Aura Roig (Metzineres, Barcelona), and Daniela Sefora Goeieman (gender-focused responses). The common thread: how to design care when, for many women, care itself is criminalized.
Meanwhile, MacDonnell faces the camera, ready to explore what often lies just outside the frame: the meaning of care when it becomes a legal risk; the price a woman pays for seeking help; and how danger is divided between legal and everyday life.
The background is cold; the necklace, warm. Between them stretches the subject at hand: a territory of decisions that cut across bodies, schedules, and borders. Here, now, the world fits inside a rectangle of light. And yet it widens when someone smiles before saying what matters.
When gender enters the frame, the map rearranges. In much of the world—including Africa—harm reduction is still designed for a generic “user.” Once you bring in a gender lens, specific barriers and responses surface: violence (including intimate-partner violence), motherhood and caregiving, sex work, police harassment and prisons, sexual and reproductive health and rights. Access and setting shift: women-only spaces, childcare, specialized support for survivors of violence, naloxone on hand, lower-risk nicotine alternatives, pregnancy- and postpartum-friendly services, and legal and social support.
The diagnosis is clear. Gender-responsive services are beginning to take root, patchily, to fill a historic void, but recognition of that need in Africa is moving far too slowly. In 2023, a core of professionals and activists chose to converge, to make visible the obstacles—violence, stigma, motherhood under suspicion, police, prisons—and to show the community work already keeping people alive. That gathering offered a stage for models adaptable to different African contexts and, above all, for the conviction that no policy works unless it first listens to those who need it.
Out of that listening came the African Women in Harm Reduction Group (AWHRG): a platform for conversation, collaboration, learning, and resource-sharing among African women involved in harm reduction. Its project is as simple as it is radical: to break silencing cultural norms, dismantle the stigma attached to drug use, and prioritize real supports for those navigating consumption in conditions of vulnerability. The agenda is practical—joint advocacy, resource allocation, funding pathways—and also political: to build effective, inclusive services that answer specific needs, not a generic “user” who never existed.
The webinar, available on YouTube, begins there, in that rectangle of light where a smile signals that, at last, the conversation is turning toward those who usually fall out of focus. And it leaves the next question on the table: how does that agenda hit the ground?
Cape Town: Prologue in a Storm
The screen trembles slightly, as if the wind were gusting through the fiber-optic line. “Welcome from a cold, wet, stormy Cape Town,” Julie says, and the weather turns into a prologue. This isn’t meteorology; it’s the atmosphere of work usually done against the wind. She thanks the honor of moderating “this important session,” among colleagues and friends, and sets the compass at the origin: the spark jumped at a panel during the 2023 African Drug Policy Week, when it became clear there was something urgent that didn’t fit the usual repertoire.
Julie names it without hedging: it’s not enough to talk about women who use drugs; services must be rethought to actually include them. Harm reduction cannot be confined to opioid substitution therapy (OST) or needle exchange.
Seen through women’s eyes, the catalog widens: link to sexual and reproductive health and rights; strengthen perinatal harm reduction; address gender-based violence; work with the police so it stops being an obstacle and becomes an ally. The list sounds technical, but underneath it beats a fundamental question: what does it mean to care when care is criminalized and the clock is running against you?
The plan also changes scale. This is the first of four seminars, covering South Africa today, with East, West, and North Africa to follow. The promise isn’t univocal but collaborative and contextual: share lessons, navigate challenges, and improve African women’s lives while respecting traditional practices and cultural codes. It isn’t a cosmetic turn; it’s a matter of architecture. Julie thanks Harm Reduction International (HRI) for “putting Africa on the map,” and in doing so, highlights the flip side: if it has to be put there, it’s because it’s often missing.
There’s also a bridge between continents. “We’ll hear from Aura Roig—introduced as the founder of Metzineres—to understand how a service designed for women in Barcelona has modeled good practices worth replicating.” The mention works as a mirror: if a European city managed to build a gender-focused harm-reduction refuge, which parts of that model can be translated—carefully and without reproducing colonial dynamics—to Cape Town’s neighborhoods, the Overberg routes, or peripheries that don’t appear on maps? From that question, the seminar’s architecture turns into an itinerary: from Barcelona to Tshwane, from the Global North to the streets where care usually arrives last.
Logistics is political, too. There will be room for questions. She asks that they be saved for the end or dropped in the Q&A box; the moderators will sift them and respond in the closing. In a world where so many women are made to justify their bodies before their words, reserving time to listen is a decision, not a formality.
Then Julie opens the first door of the story: “I want to introduce our first speaker.” Not a podium expert, but embodied experience: a woman with lived experience of drug use in rural South Africa. She names her—Caron Mathews—and adds the detail that changes the camera angle: a former community health worker, now a network leader in Genadendal (meaning “Valley of Grace”), on the Overberg periphery (Western Cape), through the STAND (Social Transformation Action Defined). It isn’t a glittering project; it is momentum assembled shoulder to shoulder. With minimal resources, they widen the circle and convert scarcity into movement—in other words, not a house patched with borrowed nails, but a canopy raised by many hands.
That’s how the webinar begins: with a city lashed by a storm, a script that refuses to repeat formulas, and a voice reminding us that harm reduction, if it isn’t centered on gender, doesn’t reduce what hurts most. From here on, the conversation moves from categories to bodies. And bodies, when they speak, usually improve the theory.
Caron Mathews: Trust as Infrastructure
Caron Mathews speaks without notes, trusting the body to remember what the page forgets. ‘I didn’t prepare anything—I’m just going to speak,’ she says, and the tone clicks into place: honesty without adornment. She’s spent years shoring up a network in Genadendal—an agricultural heritage town in the Overberg—and she starts not with metrics but with a private fracture: trust. ‘I didn’t have any,’ she admits. Her voice shook; her eyes slid away; stigma had taught her to shrink. The group taught her another grammar: stand up, take up space, ‘take what’s ours and use it.”
The word stigma keeps returning—not as an academic concept but like a door slammed in your face. In Genadendal, she says, women who use drugs avoid even stepping outside; to look for work is often to walk toward a humiliation you can see coming. That is where STAND—together with Julie and Stacey Doorly-Jones, the organization’s founder and chief executive—practices a kind of intimate engineering: workshops, conversations, a spare net woven with threads of self-awareness. In her telling, harm reduction begins there: learning to see yourself again as a whole person.
“Now it’s better,” she repeats, and the adverb opens a window. Better for going out into the street, better for presenting themselves to the community as normal women, better for speaking about what they do and what they’ve learned.
Trust—an intangible—turns into social technology: it makes it possible to go to the clinic regularly, to negotiate with the police and with health workers, to handle conflicts without becoming the conflict. She puts it in practical terms: in recent weeks, there have been no complaints at hospitals or police stations; only one woman in the group—ill—needed help to be admitted. “And everything went well,” she says, as if well were a modest and hard-won goal.
Meanwhile, life insists. Genadendal is almost indistinguishable from the fields: when the season comes, farms need hands in the packing houses, in the greenhouses, wherever summer demands. Several women, she says, dared to show up and took the shifts. It may seem minor, but here it’s a major event: employment as proof of belonging, a provisional pact with a community that, until yesterday, shut them out.
One line refuses to blur: economic fragility. “We don’t have as much of a platform as other groups,” she concedes. There’s no budget to do the work with autonomy. The verb to do hangs there, heavy with urgencies: transport to reach the clinic, mobile data to respond to an overdose, a place to meet without asking permission. Poverty—a constant reminder—isn’t a backdrop; it is policy seeping through the cracks of every daily decision.
Even so, Caron keeps returning to gratitude. She thanks Julie, she thanks Stacey, she thanks the group. It isn’t a ritual. In places where criminalization turns care into suspicion, gratitude is the modest way to acknowledge the existence of a network. That they are not alone. That help can’t be reduced to initials—OST, NSP—but to people who stay on the phone when the afternoon turns uphill.
What takes shape in her account is a plain, resonant equation: self-esteem + connection + access. No heroics; none required. Gender-centered harm reduction, in an agricultural town in the Western Cape, begins with a woman who finds her voice again and, on the other end, someone who listens without judgment. The rest—the relationship with the clinic, dealings with the police, seasonal work, a sick friend’s admission—are rehearsals of normalcy in a place that has said the opposite for years on end.
Caron closes without grandiloquence: “I’m happy to be the group’s leader… we support one another.” It may sound small to headline-chasers, but here it amounts to an entire program: shared leadership, mutual aid, small, sustained gains. Sometimes public policy fits inside that sentence. Sometimes what changes a life isn’t the law in the official gazette but the first time a woman crosses the square without lowering her gaze.
Julie’s thanks for Caron’s presence isn’t a closing; it’s a hinge. She thanks “the courage to be vulnerable before three hundred people,” and by naming the number, she turns emotion into data: here, vulnerability is a public choice. “May that fragment of life,” she says, “help explain why so many keep at this.” Not applause; an invitation to look more closely.
Then she sharpens the focus: gender-based violence in the rural areas where Caron lives is high and persistent. Julie underscores it like someone sticking a pin in the map so the exact site of the pain won’t be forgotten. Jobs are scarce, she adds—not only there but across other rural parts of South Africa. The sentence is dry, deliberately unadorned; it leaves room for Caron’s scene—the shame, the stigma, the clinic, the sick friend—to resonate without paternalism.
She also sketches the outline of what’s next: They will share the concept note for this seminar series and announce the consolidation of the HER Movement—a commitment to gender-centered, inclusive harm-reduction services. The name carries both device and intent: HER names the person historically kept from the center of design. The implicit promise is to abandon the “generic user” and build, instead, a service with a name and a body.
Kalvanya Padayachee: Founding a Common Home (AWHRG)
Kalvanya Padayachee takes the floor as if drafting a founding charter, but with the urgency of someone who knows every delay has a face. She explains that the African Women in Harm Reduction Group (AWHRG) is a common home: a place to converse, collaborate, learn, and share resources among African women involved in harm reduction. It isn’t another acronym for the archives; it’s a platform built to put at the center those long consigned to the margins; to surface evidence-based programs and good practices adapted to African contexts; and to break cultural norms and stigma that have pushed so many out of services. It will also—she adds—be a space for joint advocacy, resource mobilization and allocation, and financing, with particular attention to younger women.
She maps the work ahead and, in doing so, restores edges to words worn smooth: address concrete problems; name the specific challenges faced by women in this field—and by women who use drugs; unsettle the comfort of those who still believe that straying from “traditional” femininity deserves punishment. She frames stigma as a crossroads where gender and class overlap and where, too often, help becomes suspect. AWHRG—she insists—exists to converse, collaborate, learn, and share resources; to center women (including younger women); to coordinate advocacy, direct resources, and open funding channels. All of it while distinguishing “traditional” harm reduction—and its Global North models—from an approach specific to women in Africa.
The platform, she stresses, will not be a bulletin board. It aims to identify and spotlight evidence-based practices designed and implemented on African terms. To do that, it will need to break the norms that enforce silence, root out stigma, and prioritize support for those navigating drug use under conditions of vulnerability. The verb she chooses is exact: to offer—to offer care, to offer accompaniment, to offer routes that do not begin in judgment.
One emphasis sharpens the angle: youth. Young people are not a target audience; they are protagonists. Education and empowerment are infrastructure, not slogans, so nothing hinges on the luck of a volunteer or the whims of a fickle donor: stable networks, continuous training, and young people’s active participation in design and implementation.
She then lays bare the system’s inner workings: joint advocacy, resource allocation, and financing opportunities for African women in harm reduction. And a warning best heard without defensiveness: recognize the differences between “traditional” and Global North harm reduction and harm reduction specific to women. Not to pit them against each other, but so both are acknowledged and sustained—each in its own context, without copy-and-paste templates that don’t fit.
She closes where she began: this platform is essential to meeting singular needs through collaboration, advocacy, and resource sharing. The goal isn’t a fancy slogan but a verifiable result: effective, inclusive services for women in Africa. Underneath it, she proposes a shift in pronouns from “they need” to “we build.” That’s where the story begins to change.
Julie smiles and shifts register: “Dimakatso is the youngest on our panel and a member of the HER Movement.” She brings her onstage with a blend of pride and expectation. What Dee Nonyane is about to share, she says, is the community work underway in Gauteng: a web of active sites operating in Tshwane—proof that harm reduction can be inclusive when it’s designed at ground level, where theory trips over life.
Before handing her the mic, Julie sketches the professional track record that gives that promise its footing. Dee has been a clinical associate with the Community-Oriented Substance Use Programme (COSUP) since its launch in 2016; she pairs clinical practice with postgraduate training in psychology and now leads capacity-building. Behind the title lies a key verb: to train. Under her coordination, COSUP has trained health-care staff, community agents, and local actors—the real constellation that, when it works, keeps a clinic visit from turning into defeat.
Julie adds that Dee has designed and led national workshops and has published as a co-author on advances in the field. She isn’t reciting a résumé; she’s underscoring that practice becomes knowledge when someone takes the time to write it down and share it.
In this field, documentation is a form of care: what’s written doesn’t vanish when teams change or a funding line runs out.
There’s an ethical insistence as well: person-centered care. In Julie’s voice, it doesn’t land as a slogan but as an operating principle: treat dignity and well-being as design conditions, not decorations. Hence, the chain that links clinic, psychology, workshops, publications, and territory: a way of saying that harm reduction requires multiplying points of entry until they are many—and close at hand.
“We’re very grateful to have our little Mighty Mouse today,” Julie jokes, affectionately—a nickname that, far from belittling, points to the mismatch between size and impact. At bottom, it captures the panel’s thesis: small teams can move large structures when the strategy is sound and the work is done with the community, not on top of it.
And then, yes: the floor goes to Dee.
Dimakatso Nonyane: A Clinic in Step with the Neighborhood
Dimakatso (Dee) Nonyane begins as if unfurling a blueprint on the table: “We’re a community program born in 2016.” From there, the thesis: take health to people’s homes—where life is lived, survival is engineered, and, sometimes, defeat is too. Community-oriented primary care (COPC) aligns with harm reduction principles, and from this foundation, the program takes shape: a public, municipal initiative in partnership with universities, with a clear mandate: to bring the clinic into step with the neighborhood.
She says it without jargon, but it’s pure technique: if risk takes shape in everyday life, care has to take root where life happens. Not in the solemn building, but in churches, community halls, and borrowed rooms—places that allow a holistic approach: health, relationships, paperwork, cooking, time. Recovery, she cautions, isn’t a solitary feat; it either becomes a collective task or it fails in silence.
Hence, the support groups, the conversations with families and neighbors, and the community dialogues in schools, clinics, and workplaces. Harm reduction stops being a service and becomes a web of conversations that holds someone up when everyone else lets go.
She then lays out the minimal team that keeps that web working: peer educators—the indispensable bridge between site and participants; community health workers (here, care coordinators) who anchor care in the territory; social workers for individual and family psychosocial support; and collaborating physicians for what hurts—and for what, if left unattended, kills. No glamour: just clear roles which, together, keep a visit from ending in stigma or a shut door.
They’ve measured—not to stockpile charts, but to find out whether the method works. The results point the right way: improvements in well-being, family relationships, health, knowledge of services, and daily functioning—even where use remains chaotic.
But after the list comes the honest discomfort: who are we reaching?
In the last fiscal year, women and trans women accounted for 24 percent of those reached. The number is an alarm without a siren. If proximity is solved—nearby sites, humane hours—what other barriers remain? Fear of police? Childcare? Controlling partners? Service windows incompatible with people’s everyday economies? The question hums like a pedal note: access exists, but not equally for all.
The response begins to take shape from below: gender-based violence campaigns by and for women who use drugs; support networks among women—mothers, neighbors—who listen without pointing fingers; nutrition groups; book clubs (one started by Michelle, Dee says—the detail matters because it names a concrete leader); yoga in courtyards and halls; contemplation groups in homes to restore dignity where shame had settled.
These aren’t “activities”; they are micro-infrastructures of life.
Each one pushes back a little against the void.
Dee pauses to honor the women on the front lines. Not as symbolic homage but as operational recognition: they keep the care apparatus standing when the budget wobbles or politics looks away.
She’s grateful for a women-centered platform not out of enthusiasm alone, but because it enforces accountability: “it keeps us in check,” she says, and points to the next step. What would it take for that 24 percent to look like the real world? The question remains open, a door at the end of the hall.
In her telling, the program boils down—jargon-free—to an equation: proximity + peers + community + constant verification. A simple formula for a complex problem.
And perhaps that’s the power: when care moves to where life happens, the statistics start to look like the people.
Julie takes a breath and lets the silence do its work.
“What more can we say?” she offers, and the praise doesn’t ring hollow: this “is at the heart of harm reduction.” Not just numbers—people. Not just indicators—principles. Compassion, applied to those carrying heavy burdens of vulnerability.
She thanks in the plural—“I’m speaking for everyone here”—and leaves a compass on the table: thank you for reaching those the system does not. Then she announces a shift in latitude: “With that, I’ll hand it to our representative from the Global North: Aura.”
Aura Roig on Metzineres: Translating Care, Community as a Safety Technology
She introduces her the way you would present the keystone of a method.
Aura Roig—an anthropologist with a master’s in criminology and sociology of the penal system, and a Ph.D. candidate in medical anthropology—comes to share the guiding principles and the work behind Metzineres in Barcelona, Spain. This isn’t just another center; it is, Julie says, the first nongovernmental cooperative devoted to creating protected environments for women and gender-diverse people who use drugs, survivors of violence, and others facing multiple vulnerabilities.
Beyond directing Metzineres, Aura serves as an international advisor on drug policy, harm reduction, human rights, and gender mainstreaming: she conducts research, designs services, implements, monitors, and evaluates. Her map of work stretches beyond any single city—in Spain, the United States, Canada, Colombia, Costa Rica, and several European countries. The résumé isn’t a display case; it’s a reminder that models travel but must land carefully—adapted to neighborhoods, languages, schedules, and fears that are not always the same.
Julie doesn’t suggest a model to “copy”; she says “learn.” The promise is implicit: take from Metzineres what works—safety as a starting point, low-threshold access, a trauma-informed lens, peer leadership—and translate it to South African ground without exoticism or shortcuts. The camera returns to the shared screen. It’s Aura’s turn; from here, practice speaks from within.
Aura shares her screen, thanks the room, and thinks aloud: “Care coordinator,” she says, “I’m taking that with me.” It isn’t mere politeness; it acknowledges that language shapes practice. She thanks Caron and the African women’s network. And she positions herself with surgical honesty: she speaks from European privilege, aware of the colonial history that sustains it.
Barcelona, she recalls, was in the 1980s a city with sky-high overdose rates among those aged fifteen to thirty-five, and HIV as an open wound. The difference, she says, wasn’t heroics but policy: in Catalonia, every party agreed to invest in harm reduction without turning it into a partisan weapon. That consensus allowed a care network to take shape over time—methadone, needle exchange, cannabis social clubs, drug checking (operational since the late 1990s), supervised consumption sites (from 2003)—and, later, the ecosystem that would give rise to Metzineres (2017). It didn’t spring from a whim but from a long conversation among researchers, administrators, and people who use drugs: a mixed group that traveled, compared, and brought back pragmatic fixes the government was willing to hear.
And yet, in 2016, a limit came into view: women and gender-diverse people weren’t getting through. Not only to harm-reduction services, but neither to anti-violence networks, mental health, or housing. Having “a great system” didn’t guarantee access. If you don’t touch the structural causes of violence and exclusion, she cautions, looking only at drugs can entrench vulnerability. They were no longer dying of AIDS or overdosing at 1980s rates, but they were dying younger than everyone else—“about fifteen years less,” she says carefully—because of the street, isolation, clinical neglect, and social abandonment.
Out of that diagnosis came a movement: for nearly two years, women who use drugs met to imagine what they wanted to build. When some funding arrived, they stood it up. Metzineres was founded in 2017 as a nonprofit cooperative to create safer spaces through a holistic, person-centered approach, integrating the solidarity economy into services that had become overly institutionalized and medicalized, often disconnected from real life. And a conceptual turn: don’t put drugs at the center. “Everyone uses drugs,” Aura reminds us; the difference is whether you buy them at a bar or in an illegal market. When the substance stops occupying the core, the real problems come into view.
According to the data Aura shared, 100 percent of the 529 women served are survivors of situational violence; many sleep on the street, lose custody of their children, engage in sex work or survival sex, and live with psychological pain. The axis shifts: each woman defines her own path to well-being—physical, psychological, everyday—and the service accompanies rather than imposes a trajectory.
That requires removing barriers not only within Metzineres but across the surrounding systems. If women seek help and there’s nowhere to refer them, the service stalls—absorbing everything the wider system refuses to handle. Hence, the double task: low threshold and safety inside; outside, seeding a harm-reduction lens so mental health, housing, justice, gender-based violence services, and social services adopt these practices. Always with safety and consent: not every political arena is safe for women who have never spoken in public; their voices must be written into plans and policies without exposing their images or aims beyond their control.
The material portrait punctures any idealization. There is no building; there’s a double garage. Inside: safer spaces for different modes of use; beds for rest; workshops—cosmetics, trades; and an everyday diplomacy with the neighborhood cooked into Friday paellas: “you win a neighborhood through its stomach,” she smiles. A legal accompaniment service tailored to women rounds out the offer. There is also a unit for monitoring, planning, and evaluation, with new metrics designed to measure what matters but is often overlooked in standard reporting.
UNODC (United Nations Office on Drugs and Crime) has recognized the experience as a good practice and left the door open to continue developing the work and its materials.
Beneath the inventory runs a plain ethic: center women and gender-diverse people under conditions of safety; without fetishizing their presence; and build community as a health technology.
What Aura offers isn’t a recipe to copy but a method to translate: listen, adjust, and redistribute risk and power until the system stops pushing the same people to the edge.
Daniela: What Holds, What Casts Out, Data That Care
On screen, Daniela Sefora Goeieman appears, her voice calm yet firm. The webinar timer reads 36:20, and something in her presence—patient composure—signals that what follows won’t be a mere technical report but a committed, embodied account of what it means to research—and to resist—from a woman’s body inside a health system that so often fails to listen.
Daniela is no stranger to the community or to the social pain that runs through it. She is a clinical associate and an associate professor in the Division of Clinical Associates, yet those solid titles only skim the full scope of her work. She trained at the University of the Witwatersrand (Wits) in Clinical Medical Practice and later deepened her focus on addiction care and Family Medicine (St. Ambrose University).
It’s no accident that her passion for teaching began in 2018—not in a high-ceilinged lecture hall but in the field, teaching public health to community workers. There—in that contact without hierarchies—her vocation began to take the shape of a manifested ethic. For Daniela, teaching is not merely the transfer of knowledge; it is a lived commitment alongside those pushed to the margins of policy, budgets, and medicine’s official story.
Her voice doesn’t waver as she states her aims: to integrate addiction care—comprehensive, dignified, effective—into primary health systems. And she goes further: to protect children. In that gesture, an ethic unfolds that holds together the intimate and the structural. Because to speak of public health without speaking of care, gender, childhood, trauma, and community is to repeat formulas without a pulse.
Daniela doesn’t theorize in the abstract. She wants her work—academic and personal—to have tangible effects: policies and interventions that are not only evidence-based but also literate in culture, accessibility, risk, and context. Above all, literate in humanity.
She begins, and the first thing we hear isn’t a declaration but an apology. The connection—like so many other infrastructures in South Africa—flickers. “I hope you’ll hear me clearly for the time I’ve been given,” she says; and though she’s naming a technical issue, the line lands as a metaphor: the struggle to be heard in a system that rarely listens to women who use drugs or to those who care for them.
What she lays out in the next minutes isn’t just a results presentation. It’s an intimate account, threaded with the doubts of a young professional who, in her early years of practice, supported women using opioids in opioid substitution therapy (OST) without yet having all the answers. Some became pregnant during treatment, and she—still in training—had to face urgent questions: what does it mean to care in these contexts? How do you protect a woman when the system, even in its therapeutic intent, reproduces exclusions?
That was when the COSUP model—the Community Oriented Substance Use Programme, shaped by harm-reduction philosophy—began to take shape as an institutional response, but also an emotional and political one. Because, as Daniela reminds us, good intentions aren’t enough. We must produce data. Look. Listen. Name. And, above all, not romanticize intervention in the absence of evidence that safeguards those involved.
The presentation stalls: the slides won’t advance. Another reminder, perhaps, that in the Global South, technology doesn’t always behave as it does in international reports. When she finally manages to share her chart, the void is stark: according to the World Drug Report, data on drug use in Africa are scant, almost nonexistent. The southern part of the continent—and with it, millions of lives—remains cartographically absent from the global drug debate.
Even so, there are cracks to look through. In South Africa, thanks to the South African Community Epidemiology Network on Drug Use (SACENDU), there are reports on people admitted for substance use. Among those under twenty, the primary substance reported is cannabis, followed by methamphetamine and heroin. But a more troubling signal emerges: a rise in people who inject drugs amid high HIV prevalence.
Women who use drugs, in particular, face multiple vulnerabilities: increased exposure to HIV, intimate-partner violence, and limited access to gender-responsive services. How do we respond when the numbers confirm what the ground has been shouting for years?
Here, a central tension in her work comes into view: how do you design truly integrative interventions if models are still built on “neutral” logics that erase gender? COSUP—innovative for offering community-based OST in South Africa—still runs up against structural challenges. The difficulty of recruiting women for studies on retention and HIV/hepatitis C prevalence is one symptom. It isn’t only methodological; it may signal that existing services still don’t meaningfully converse with these women’s realities.
The study sets a clear objective: to understand the characteristics of women who access OST. Through a descriptive–observational design, Daniela and her team analyzed electronic records and paper files, examining variables such as age, employment status, experiences of violence, and pregnancy during treatment. The findings sketch a sharp profile: a young majority (20–29), unemployed, and users of community services. One in three had experienced intimate-partner violence. Nineteen percent were pregnant while receiving OST.
The loss rates speak, too: 43.6 percent lost to follow-up and 12.9 percent returning to problematic use. On the other side, variables associated with better retention: knowing one’s HIV status, initiating OST at an older age, and receiving more than 40 mg of methadone a day. Daniela ventures a reasonable hypothesis: learning you are living with HIV can trigger a psychological shift—an impulse toward self-care—that supports adherence to both OST and antiretroviral therapy (ART).
At this point, the account takes a more political turn. Alliances between harm-reduction programs and organizations such as Harm Reduction International have made it possible to integrate HIV treatment within the COSUP model. Although that integration wasn’t the focus of the analysis, Daniela infers—with methodological caution—that such coalitions may be pivotal for improving adherence and comprehensive care.
Even so, not all women are represented. The study focuses on those who access OST, leaving out women who participate only in needle and syringe programs (NSP). In addition, the type of institution—clinics, hospitals, NGOs—may shape both care and patient profiles, a source of variation that warrants future research.
And then, the central question: so what? What do we do with this evidence?
For Daniela, the roadmap is clear: prioritize the sexual and reproductive health and rights of women who use drugs; establish active, empathetic, sustained follow-up; and start with training. It isn’t enough to upskill staff already in service: intervention must begin in the university, so physicians, social workers, psychologists, and community health promoters understand from the outset that substance use is also a social, economic, and gendered phenomenon. That behind the word “addiction” lie exclusions, unsupported maternities, accumulated traumas, and contested survivals.
The conclusion, unfanfared, leaves a door ajar.
Daniela argues for economic autonomy and a comprehensive approach guided not only by experts but by women who use drugs themselves.
This is not about speaking about them, but with them—even from their voices.
Because, as her research suggests, the most valuable knowledge isn’t always born at the margins of statistics, but at the margins of the system.
Sleepless Numbers, Open Questions
When Daniela finishes, a density hangs in the air that the webinar’s clock can’t contain. Julie, the stopwatch at her back, takes the floor again with a blend of gratitude and urgency. She thanks her, knowing that beneath the “very interesting” statistics, there are lives holding on—often alone.
“We could have spent hours unpacking these data,” she admits. But time is tyrannical in virtual spaces too, and the second hand insists on moving forward. We reach the reflective heart of the gathering: the Q&A and discussion, where certainties soften and more fertile doubts emerge.
The presentation folds; the dialogue opens. Julie introduces Colleen Daniels to guide the Q&A. “She needs little introduction,” she says, as if her record could speak for itself. And indeed, Colleen embodies a rare intersection of technical knowledge and political commitment. She is now the interim executive director and head of public health at Harm Reduction International. Her twenty-five years of work won’t fit on a list: Australia, Kenya, the Netherlands, Switzerland, Thailand, Tonga, and the United States; and among the institutions, the World Health Organization (WHO), the Stop TB Partnership (UNOPS), AusAID, and Health Action International. A life map that sharpens an intersectional, pragmatic gaze. She is also profoundly South African, as Julie notes with pride.
The floor goes to Colleen. Her task: pick up the thread of what’s been said, pull at the questions tucked into the margins of the presentations, and weave from them a shared common sense.
Because, as anyone working in harm reduction knows, there are no closed answers when the subject is bodies, inequality, and survival. Only better questions—clearer, more human.
What Women Say When No One Interrupts Them
When Colleen begins, her voice doesn’t step into a conversation; it opens a window. She thanks the speakers with genuine warmth and makes it clear that what’s been said isn’t just important—it’s urgent. “It’s been extraordinarily revealing,” she says. But the most revealing thing isn’t always the answers; it’s the questions that keep buzzing afterward.
Colleen doesn’t dwell on technicalities. She says the obvious—and rarely this plainly: hundreds of millions of people use drugs worldwide. Some struggle with their use; many do not. All should be able to access harm-reduction services if they want to. Because harm neither begins nor ends with the substance, it begins with stigma, exclusion, poverty, and violence so normalized that it becomes invisible.
She pauses. She speaks from her work with women who use drugs in different countries. And the axis shifts: when she asks what they need, they never—never—ask for methadone or needle exchange. What she hears is another list, more elemental and fierce:
— I need food.
— I need a home.
— I need a job.
— I need to know my kids are okay.
— I need to be safe.
How do you talk about naloxone when there’s no bread?
How do you ask for treatment adherence when a woman is afraid to go home because violence is waiting for her there?
What Colleen sets on the table isn’t an attack on the biomedical frame, but a statement of its limit. And that limit becomes a call: change perspective, shift the center, demedicalize the idea of care to understand that well-being—well-being, as Aura once offered in an offhand conversation in Bogotá—is integral, communal, situated. What we need, she says, are centers of well-being, not only health centers. And what Daniela, Dee, and Caron laid out are, at bottom, seeds of that: programs that know no one saves herself alone; that community isn’t a bonus but the core of care.
As she speaks, the chat floods with questions. The team whispers that time is short, but Colleen gives herself to the productive chaos of exchange.
She reads an anonymous query aloud: Do services include sexual and reproductive health and rights? The answer is yes—at least in Aura’s and Stacey’s programs—and she promises links. Then, laughing, she allows herself an aside: “Menopause! I need reading glasses now—it’s ridiculous,” she jokes. The bodily, everyday confession breaks the antiseptic script of so many seminars—and doubles as a sharp critique: why don’t we talk about menopause in harm reduction? Why are perimenopausal symptoms in women who use drugs so often misread, pathologized, or mistreated?
The next question goes to Dee: What’s the most common reason women use drugs? Colleen, with elegant firmness, sidesteps the trap. “I don’t think we need to know why people use drugs.” Then the disarming line of political clarity: “We use drugs because we like to. Because we need to. For whatever reason.”
With that, she shifts the center of gravity. This isn’t about pathologizing desire or moralizing use; it’s about building environments in which decisions—including the decision to use—are not lived from precarity or fear. Where desire need not be, necessarily, an escape route.
Knowledge from Below: Plants, Care, and Shared Epistemologies
When Colleen opens the floor, the conversation moves like an underground current finding cracks through which to surface. Dimakatso (Dee) Nonyane answers first, with the precision of someone who knows her terrain inch by inch: the program is active in four regions of Tshwane, and she’ll share a leaflet with addresses and contacts. A brief, administrative reply—but necessary. Because, as with any serious public policy, the concrete matters: where’s the door? Who do you call? Who do you turn to?
Without missing a beat, Colleen turns to Aura, picking up a question from Yolande Jordan. It strikes a raw, almost philosophical nerve: does Metzineres also acknowledge the potential harms of cannabis when it’s used as a harm-reduction tool?
Aura doesn’t hesitate; she’s walked this road before, but chooses to return to it not with defensiveness, but with pedagogy. “Yes, we recognize the risks,” she says. “But the starting point lies elsewhere: listen to women. Don’t theorize about them. Don’t define them from the outside. Listen.”
What they saw at Metzineres wasn’t blind or unbridled use, but a sequence of everyday decisions—sometimes precarious, sometimes deeply deliberate—about why and how to use cannabis. To quiet anxiety? To sleep? To bear physical or psychic pain? To steady hunger or loneliness? At what times, at what pace, and under what conditions?
The method was simple and radical: document what women said—no filters, no moralizing, no ranking. Then bring that tide of testimony into conversation with academic knowledge. They searched the scientific references. They spoke with José Carlos Bouso, scientific director at ICEERS (International Center for Ethnobotanical Education, Research and Services), with Mujeres Cannábicas, and with cannabis specialists.
The not-so-surprising surprise was finding that what women knew from experience had counterparts in the scientific literature.
The wisdom was there, only scattered—encapsulated in journal articles that almost no one outside academia would read, least of all those at the margins of exclusion.
So Metzineres did what any committed science ought to do: translate. Not only into accessible language, but into the material, emotional, lived, and cultural context. And they layered scientific knowledge onto popular knowledge—not to replace it, but to confirm it, strengthen it, and dignify it.
“And that,” Aura says with quiet force, “is harm reduction.”
Colleen, in her quick, agile style, offers brief thanks and moves to a new question, this time from Ruth Bergen, directed to Daniela and Dee:
“Are women with opioid dependence required to be on opioid substitution therapy (OST) in order to access antiretroviral therapy (ART) at COSUP centers?”
The Borders of Access: Conditionalities and Silent Exclusions
Daniela answers with the steady calm of someone who knows the system’s backstage: no; being on OST is not required to access ART (ARVs) at COSUP centers. Not for women, not for men, not for nonbinary people. It isn’t required. And that clarification—apparently technical—is in fact profoundly political: it sketches the borders of access.
In public health, whoever defines access ends up defining exclusion as well.
She anchors the point in lived experience: at a clinic where she worked the day before, she watched women come to COSUP and to the public health network without enrolling in any substitution protocol. Moreover, COSUP doesn’t serve only people who use opioids; people arrive with methamphetamine, cannabis, and other substances. The service isn’t organized by molecule but by need.
The distinction matters.
In too many settings, services are designed around the molecule, not the person, as if the clinical response followed a pharmacological taxonomy instead of a life in motion. Daniela dismantles that logic simply but forcefully: care should not depend on the type of drug, but on the conditions—social, economic, and relational— that surround its use.
A thornier question arises: how do you approach family reintegration for people who use drugs when they’re seen as “failures” or as the source of their families’ suffering?
The question opens both an ethical and a practical fault line. Silence opens for a beat. Not because answers are lacking, but because the question is also a wound.
Colleen takes the floor as few can: not to answer, but to dismantle the frame. What needs changing isn’t only services, she says, but language, narratives, the way we talk about—and therefore think about—people who use drugs. “The perception that they’re failures…,” she repeats, and lets a cutting pause fall. That perception is born of stigma, structural discrimination, and a moralizing model still dominant in too many health policies.
Then she releases a line with a scalpel’s edge and political clarity: “At the end of the day, we’re all people who use drugs, one way or another.” What shifts, she adds, is the state’s seal of approval. Some uses are legalized, legitimized, and even celebrated (alcohol, caffeine, prescription anxiolytics); others are criminalized and pathologized. The split isn’t evidence-based; it’s built from history, politics, and, often, colonial logics of control.
If we truly want to talk about well-being for women, girls, trans, and gender-diverse people, we have to talk about community response. Diagnosis isn’t enough: we must transform the language, the practices, and the affections that hold people in—or push them out. The invitation is not only to respond, but to think again, from another place.
Unlearning Fear, Relearning Care
Dima steps in without hesitation, with the conviction of someone who inhabits health—through the body, through relationship—and says something as simple as it is radical:
“If you’re not responding from fear, you’re not doing enough.”
That’s the script families inherit. But once they’re released from that panic— from wanting to be fearful—they are free to love their relatives again, free to set their own boundaries, free to say: I still love this human being, regardless of everything we’ve been through, and to reconnect. All we’ve inherited has created such panic that families no longer know how to relate; the idea that ‘if I’m not fearful, I’m not responding with enough intensity’ must change. “Thank you,” she ends.
The cultural inheritance of fear has seeped into how we relate to one another. It taught us that unless we’re afraid, we’re not doing enough. That pedagogy no longer serves. It’s time for another: a pedagogy of connection, mutual recognition, and informed care—a practical, affective literacy that allows us to accompany without punishing, to support without controlling.
Prohibition: When Context Becomes a Trap
Aura picked up the thread with quiet force. She agreed with the previous speakers but sharpened the point: in her view, the issue was not drugs but prohibition, stigma, and discrimination.
She shifted registers, acknowledging the European privilege that shaped her path: she had been educated in harm reduction, had reliable information and access to drug checking, within a caring community. For her, these were everyday harm-reduction strategies—ordinary ways people avoid harm.
She went on to argue that most harms do not arise from use itself. Some patterns of use may be unhelpful, she conceded, but risk multiplies when someone must travel to an illegal spot and be exposed to police; when work is out of reach, survival may push people toward theft or other illegitimate means. In that light, the problem lies elsewhere: drugs may be a problem—or not—depending on context.
She offered a familiar analogy: driving is safer when one is trained, when signs are clear, and when the seat belt is fastened, yet crashes still occur because others are untrained or signals are missing. We don’t ban cars on that account. What matters, she concluded, is the quality of information and the strength of the care network; in a word, community.
Who Produces Knowledge —and From Where
And then, as if closing a loop, Daniela returns. This time, the focus shifts from data to reflecting on the origins of knowledge. She recalls earlier work with children as researchers and, from there, poses a radical question: what counts as valid knowledge, and who has the right to produce it?
Addressing—perhaps—the academic audience, she points out what is so often omitted: research is shot through with power. What ends up labeled “rigorous data” or “serious policy” usually springs from external, aseptic, hierarchical gazes—ways of looking that study without listening, extract without engaging, and publish without accountability to those whose experience supplied the raw material.
Hence, she says, the urgency of a paradigm shift: women who use drugs should not be merely objects of study, but researchers and producers of knowledge. Knowledge should be built collaboratively, from an ethic of mutual recognition—not from academic extractivism.
“We can’t keep entering communities saying we already know, already analyzed, already have the answers.”
We must break with that mindset, that philosophy, that personal narrative we’ve often never examined. Revisit our beliefs; revisit our ways of seeing. Only then, perhaps, can we produce knowledge that is not only accurate but also just.
Colleen listens. At this point, she’s no longer moderating; she’s tending. With the sensitivity of someone who has walked through too many policy rooms and too many soulless statistics, she brings into view what is almost never named: pregnant women who use drugs.
She recalls the irreparable harm of the media script of the eighties and nineties, when the term “crack babies” took hold in the United States—words that not only stigmatized but also criminalized and controlled the bodies of poor Black women. Words that became policy. Policies that became a cage. That script crossed borders, and what began as propaganda hardened into protocol in far too many places.
So Colleen invites Julie to share a recent initiative: a toolkit for health professionals who work with pregnant women who use drugs. Julie explains that the material—developed with support from the Elton John AIDS Foundation and Sanford Health organization—is evidence-based, adapted to the African context, and will be officially presented in a webinar on August 28. She adds that it carries the backing of the Perinatal Harm Reduction Academy and the Harm Reduction Coalition.
Beyond the technical achievement, something else appears: a will to rebuild care from what was ignored.
This isn’t only about clinical guidelines; it’s about recognizing the dignity of those systematically rendered invisible—and writing that dignity into procedures, budgets, and practices, so that motherhood is not turned into suspicion again.
Radical Tenderness: Strategy, Method, and Right
“We’re Only Just Beginning… and Already We Have to Stop”
With that line, Colleen says what many were thinking and no one had voiced. And yet her final turn doesn’t close things; it opens them. She invites a rethinking from the roots. Because in Africa—she reminds us—harm reduction is still emerging, and there’s an opportunity there: if we do it well now, we won’t have to repeat the mistakes of the Global North. We can avoid services nobody wants, decontextualized programs, and policies that fail before they start because they never listened to the people they meant to care for. The hinge is data: without reliable data, budgets are guessed at, programs don’t scale, needs are assumed, and then blamed. “Why didn’t it work?” donors ask. It didn’t work because we didn’t seed the ground.
Colleen goes further: loss to follow-up isn’t an individual failing; it’s a symptom of discriminatory structures. To break them, we must drop the individualist gaze imposed by capitalism—the one that loads public responsibility onto an isolated subject, detached from her social fabric—and commit explicitly to a community approach.
“I am Colleen, yes, a person. But I’m also Colleen, who lives in Tower Hamlets, in London. And that matters.”
We don’t live in a vacuum. We live in communities. And those communities can be scaffolding—or the tallest barrier.
Picking up the threads woven by Aura, Daniela, and Dima, Colleen names the symbolic heart of the gathering: radical tenderness. And she grounds it in two explicit frames: radical activism of care and radical care, held within a community approach. She says it like someone who has found a slogan that is not only political but philosophical. “I’d never seen that in a presentation,” she admits. But having seen it, she can’t stop thinking about it. Because if anything is missing from health systems, drug policy, and biomedical discourse, it is tenderness: tenderness as strategy, as method, as right; as a language that says: you matter, we see you, you belong, you are not alone.
Hence her proposal: not just data or strategy, but new ways of doing policy. A radical politics of care; programs that speak plain, human languages; that recognize the value of first-person knowledge; interventions built alongside, not from above.
It wasn’t a closing. It was a seeding. And perhaps the most powerful kind.
When the Zoom Ends: What Remains
When the cameras switch off and the microphones go quiet, more than a recording remains: an echo. A murmur in memory. A vibration that doesn’t dissolve, as if the words—the ones that unsettled, moved, illuminated—kept circulating beneath the seminar’s digital skin.
It wasn’t a technical meeting. It was an assembly of feeling, a laboratory of uncomfortable truths and possible tenderness. What was woven there—between testimony, data, and questions—composed a counter-hegemonic narrative of harm reduction: not as an exclusively biomedical policy, but as an ethic of listening, a practice of care, a form of radical resistance.
They spoke about women who use drugs and the violence that surrounds them; also about the right to use without apologizing, without hiding, without being reduced to a medical or penal category. They spoke about community as a space of care and as a system of exclusion. About the data that are missing and the budgets that fail because no one seeded the ground they’re meant to grow in. About programs designed for “those who qualify,” not for those who survive as they can.
But the most powerful—the most deeply human—thing was what was named outside protocol: radical tenderness. The kind that doesn’t show up in reports or donors’ logical frameworks. The kind with no indicators—yet it saves. Tenderness as recognition. As politics. As a methodology for re-inhabiting bodies broken by stigma, silence, and the war on drugs.
They also spoke about language: how naming is a decision; how clinical terms can objectify; how words can oppress or liberate. Colleen, Aura, Kal, Daniela, Dima, Caron, and Julie offered not just technical knowledge. They offered a new grammar for thinking about health, exclusion, and desire—a way of seeing that doesn’t split data from the body, or theory from lived life.
Perhaps that is the gathering’s most valuable outcome: producing knowledge from the wound, from experience, from listening. Dismantling the idea that knowledge is born only in universities or conferences, and affirming—with firmness and care—that women who use drugs are not objects of study but epistemic subjects, producers of meaning.
In the end, what remains is not only what was said, but what was opened: a promise to keep speaking, researching, and showing up alongside—and, above all, to keep listening. Because, as the session reminded us, if community is where harm begins, it must also be where healing does. And perhaps—just perhaps—this is the beginning of something larger.
* * *
Harm Reduction International. (2024, July 11). Gender-centred harm reduction in Africa [Video]. YouTube.









I checked the post with ItsAI detector and it shows that it's 84% generated!