28.6 Billion Cigarettes a Year
A study lays bare the UK’s map of inequalities: North vs South, working class vs privileged, quitters vs those still trapped.
It’s not just smoke. It’s a collective scar. Each of the 28.6 billion cigarettes consumed every year in Britain draws an invisible mark across the country’s body: deeper in working-class neighborhoods, fainter in the prosperous South, yet present everywhere.
The smoke doesn’t dissipate; it lingers on the yellowed walls of council flats, in exhausted lungs, in statistics that foretell shorter lives. A recent study confirms it with surgical coldness: tobacco, even in its retreat, remains a brutal mirror of who breathes easily and who merely survives in the United Kingdom.
In Britain, tobacco smoke still sketches a map found in no atlas, yet it speaks with a bluntness impossible to ignore: the map of inequalities.
Smoking is no longer a mass habit; its decline is undeniable. Yet among those who remain, the intensity has not waned: an average of 10.4 cigarettes a day, adding up over the year to 28.6 billion cigarettes. Each spark, a mark; each exhalation, a statistic. These are numbers that aren’t merely read—they are felt, like open scars. So reveals a recent study published in Nicotine & Tobacco Research, updating—with data from 2022 to 2024—the invisible cartography of consumption in England, Scotland, and Wales.
The study bears the signatures of Sarah E. Jackson, Jamie Brown, Vera Buss, and Sharon Cox, researchers at University College London and Behavioural Research UK. Names that, beyond their academic credentials, read here like those of cartographers of a country divided by smoke. Because their work did more than count smokers: it went further, toward a more intimate, almost intrusive question. Not just who smokes, but how much they smoke—that quiet measure that reveals, with the precision of a scalpel, the intensity of dependence and the potential depth of harm.
To achieve this, they delved into the Smoking Toolkit Study, a monthly survey that functions as a living archive: wave after wave, it captures the voices of more than 77,000 adults, tracing not just numbers but stories condensed into percentages. Each response is a point on the map; together, they sketch a living cartography of tobacco’s persistence in contemporary Britain.
The Portrait of the British Smoker
In Britain, the smoker is no longer a crowd. But neither is smoking a relic of the past. Only about 13.9 percent of adults sustain the habit, and they do so with an intensity that still leaves a mark: roughly ten cigarettes a day on average. There is, however, a more rigid core—5.5 percent—who cross the threshold of twenty, a figure that speaks less of pleasure than of endurance, even entrapment. These are the lowest levels ever recorded, and yet still enough for smoke to etch itself into the country’s skin.
Translated into the cold language of demography, that means 528 cigarettes per person per year. But smoke is never just a number: it is persistence. Small embers lit day after day that, when added up, become something larger—28.6 billion repeated gestures, tattooed onto Britain’s collective body.
But perhaps the most revealing detail lies not in what is smoked, but in what goes unrecorded. While estimated consumption reaches 28.6 billion cigarettes, only about 14 billion were sold legally in the UK last year. To that, one must add sales of roll-your-own tobacco, equivalent to between 4.5 and 6.3 billion cigarettes, based on estimated yield per kilo. Even so, between a quarter and a third of total consumption remains unaccounted for. This gap is far from trivial: it raises uncomfortable questions about the weight of the illicit market, cross-border purchases, or perhaps the cracks in the recording systems themselves.
One of the study’s most unsettling findings goes beyond the mere counting of cigarettes. In Britain, smokers from less advantaged classes not only consume more but also inhale more deeply and often turn to tobacco with higher nicotine content. It is a double exposure—greater quantity and greater intensity—a combination that deepens the invisible scars of inequality.
And although the study does not measure it directly, this pattern suggests that much of that unaccounted-for consumption—the portion that escapes legal sales—may be concentrated precisely within these groups, who more often turn to cheaper sources, from illicit tobacco to cross‑border purchases.
The authors explain part of this phenomenon through the concept of titration: smokers adjust their way of consuming—taking more puffs, inhaling more deeply—to keep nicotine levels in the body stable. The result is a higher concentration of cotinine, a biological marker that reveals more intense exposure, even when the total number of cigarettes appears similar.
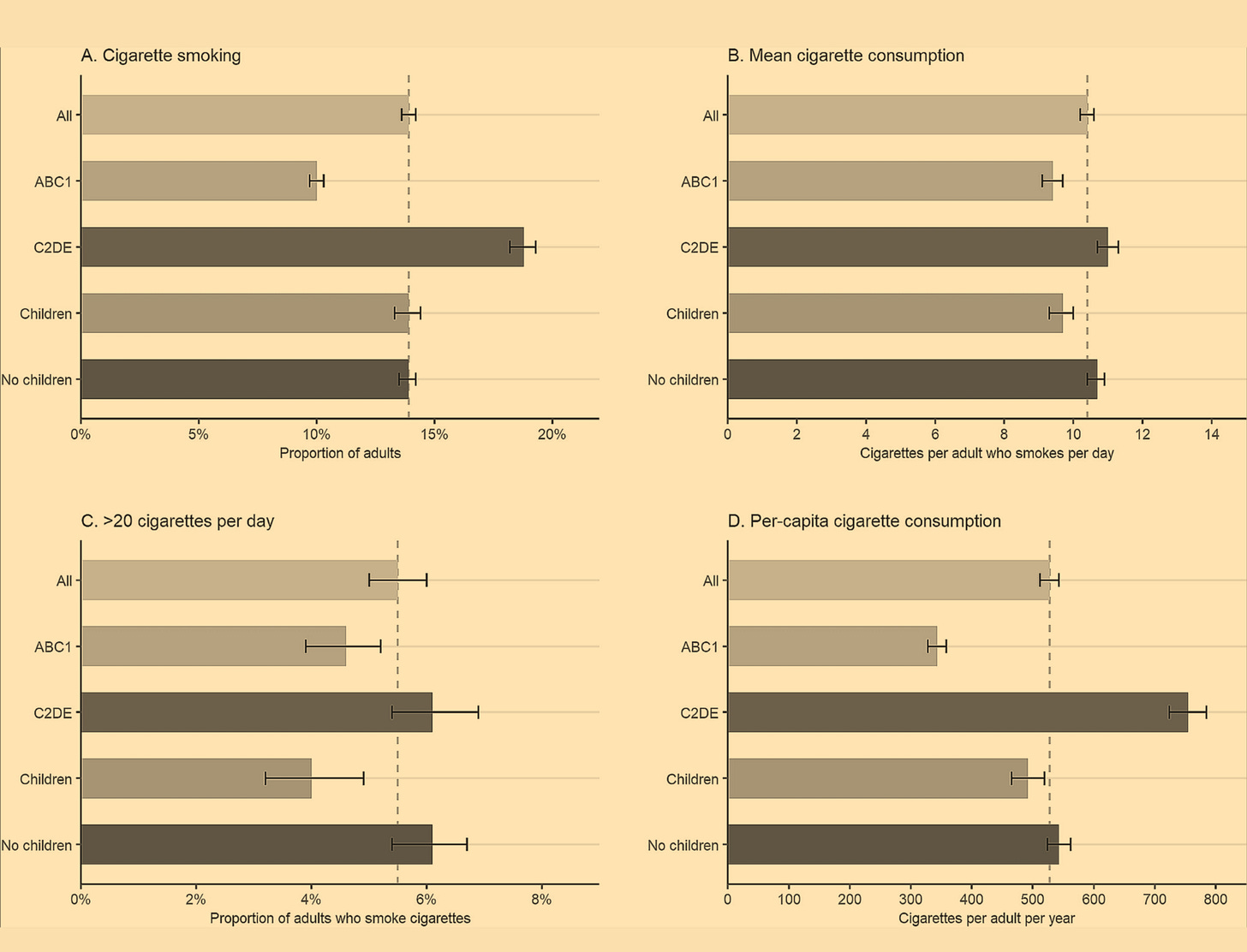
The differences are stark. In the social map of smoke, the less advantaged classes (C2DE) bear a double burden: they smoke more often—18.8 percent compared to 10 percent among wealthier groups—and light up more cigarettes each day: 11 versus 9.4. This is not just a statistic; it is evidence that tobacco, even in retreat, remains a daily reminder of the invisible borders separating those who can breathe more easily from those who can barely afford to.
Translated into annual figures, the contrast is brutal: 755 cigarettes per capita—more than double the 343 of the most advantaged. In this portrait, smoke ceases to be merely a vice; it becomes a social wound that cuts across class. Because inequality is not just a statistic—it is breathed. It lives in the intensity of the habit, in every drag that passes through the lungs of those who live with less.
On the geographical plane, the tobacco map traces the same scars the United Kingdom has carried for decades. The Northeast of England and Scotland—regions marked by deindustrialization and the worst health indicators—top the charts at 11.7 cigarettes a day, as if the smoke were also a residue of those open wounds. At the opposite end, London sketches another profile: that of the lighter smoker, averaging 8.4 cigarettes a day—a statistic that seems to speak as much of lifestyle as of unequal access to resources and alternatives.
But averages never tell the whole story. The Southeast of England, with its dense population and vast satellite cities, emerges as the true epicenter of smoke in absolute terms: nearly 4 billion cigarettes lit each year. It is a reminder that even in the most prosperous regions, tobacco remains an industrialized haze—a product of an economic machine that turns dependence into business and inequality into fuel.
Home and Tobacco: Smoking Less for the Children?
The study also paused at an intimate setting: the home, a space where smoke not only stains walls but intertwines with routines and affections. Does living with children influence the number of cigarettes lit? The data hint at a trace of moderation: those with children at home smoke, on average, one cigarette fewer per day (9.7 versus 10.7). A small, almost symbolic gesture that reveals both the persistence of the habit and the minimal, insufficient attempt to protect those who breathe closest.
But appearances deceive. When the data are adjusted for age, the difference vanishes: it is not necessarily the presence of children that dampens the habit but the fact that younger adults—who tend to smoke less—are also more likely to live with minors. The conclusion is an uncomfortable one: the home, even with children, is not always a smoke-free territory. At times, it is quite the opposite—the setting where addiction and vulnerability share the same air.
The Nearly Hidden Cost: Health, Social, and Environmental
The study does more than count cigarettes: it measures their scars. Each one carries a price rarely shown on the pack: in England alone, smoking accounts for around £2.9 billion annually in healthcare and social care costs. Translated into everyday terms, that’s about £0.12 for every cigarette lit—a silent debt paid by the public system and, ultimately, by society as a whole for each puff.
But the damage doesn’t end with the body. The 28.6 billion cigarette butts generated each year amount to roughly 140,000 tons of waste—the most common litter on the planet. Each filter, tiny and seemingly harmless, carries a mix of plastics and toxins capable of persisting for decades in ecosystems, a silent legacy the smoke leaves long after it has dissipated.
These remnants accumulate in streets, rivers, and coastlines, reminding us that smoke doesn’t vanish as easily as we like to believe. It transforms. It settles—visible or invisible—on our bodies, our cities, and the ecosystems we inhabit, extending the habit’s footprint far beyond the last cigarette.
Though the report maps Britain’s smoking landscape with precision, its authors warn that the inequalities it exposes are no local anomaly: they reflect a fracture shared by much of Europe and other high‑income countries. Here, smoke becomes a universal language, revealing where our society’s deepest wounds are concentrated.
Where poverty intersects with the habit, tobacco ceases to be a mere vice: it becomes a silent vector of inequality, a mechanism that perpetuates health gaps that public policies—despite decades of effort—have yet to close. It is the uncomfortable reminder that, on the map of smoke, the lines are not easily erased.
Thus, the British case stands as both a mirror and a warning: until the social roots of consumption are addressed, the promise of a smoke‑free generation will remain a horizon that drifts further away each time we think we are approaching it.
Closing the Class Divide: The Unfinished Challenge
The statistical snapshot reveals an uncomfortable truth: although smoking prevalence has plummeted since the 1990s, socioeconomic and regional inequalities persist like open wounds, reminding us that smoke doesn’t simply vanish as numbers fall—it festers where poverty and vulnerability sustain it.
The study’s authors warn that it’s not enough to reduce the total number of smokers; it’s equally crucial to narrow the gaps in consumption intensity. They emphasize that the most disadvantaged groups not only smoke more but are also exposed to higher levels of toxins with each cigarette.
The report doesn’t stop at diagnosis: it calls for strengthening cessation policies, explicitly tailored to the groups and regions where smoke refuses to clear. More than a mere technical adjustment, it is an attempt to suture the divide that still separates North from South and working classes from the privileged. Because in those territories and households, tobacco is more than a habit—it is the persistent reflection of an inequality that spans generations, a symptom of wounds that public policy has yet to heal.
And so emerges the question that will shape the immediate future: Can Britain achieve its dream of a smoke‑free generation without confronting the social roots that fuel it? Because the problem doesn’t burn only in the cigarettes—it burns in the inequalities that keep them lit.
The data, like the cigarette butts piling on pavements, make it clear that the answer will require far more than good intentions. It will demand acknowledging that the scars tobacco continues to etch on the country’s collective body will not be erased by isolated campaigns or political promises—they will require deep, sustained policies capable of confronting the inequality that keeps the smoke alive.
The Smoke Map in Numbers
Prevalence: 13.9 % of adults in Great Britain smoke.
Consumption
Average daily use: 10.4 cigarettes per smoker.
Heavy smokers: 5.5 % smoke more than 20 cigarettes a day.
Per‑capita consumption: 528 cigarettes per person per year.
Annual total: 28.6 billion cigarettes lit across England, Scotland, and Wales.
Social Inequality
Less advantaged classes (C2DE): 18.8 % smokers; 11 cigarettes per day.
Wealthier classes (ABC1): 10 % smokers; 9.4 cigarettes per day.
Annual per‑capita consumption: 755 (C2DE) vs. 343 (ABC1).
Geographic Map
Highest daily consumption: Northeast England and Scotland (11.7 cigarettes).
Lowest daily consumption: London (8.4 cigarettes).
Highest total consumption: Southeast England (nearly 4 billion cigarettes per year).
Economic and Environmental Impact
Health and social costs: £2.9 billion annually (≈£0.12 per cigarette).
Waste: 28.6 billion cigarette butts (≈140,000 tons per year).
Cigarette butts: the most common litter on the planet, loaded with persistent plastics and toxins.
Jackson, S. E., Brown, J., Buss, V., & Cox, S. (2025). Sociodemographic and regional differences in cigarette consumption across Great Britain: A population study, 2022–2024. Nicotine & Tobacco Research.




Another excellent blog, Claudio. Those in the lower socioeconomic class often have higher prevalence of smoking rates. Sadly, due to the UK's recent about-turn with regards to safer forms of nicotine (vaping), and insisting they are upgrading regulations, to curb youth appeal. With banning disposables, and later in 2026 taxing vaping e-liquids, even those without nicotine, as well as a possible flavour ban. These proposed draconian polices will not produce fewer smokers. If anything, it will only boost illicit supplies of cigarettes. As well as boost the illicit supply and demand for vaping products. It sends the wrong message to the public by insisting that vaping is equal to smoking. While public health advocates still insist that those who cannot quit smoking with traditional methods, vaping offers them a harm reduction alternative to quit smoking, which can spare them from smoking-related diseases related to combustible tobacco use (cigarettes). I'm sure the same graph would showcase the same results in many other countries. Those in the lower socioeconomic classes, those who identify as LGBTQ+, and those who work in service industries often have higher smoking rates. Over-regulations on vastly less risky forms of nicotine, vapes, Snus, & oral nicotine pouches just keep a population trapped in smoking. Ensuring that a set percentage of people will remain trapped in smoking habits. Public policies should always be based on science and evidence, and not based on fears or ideologies for a nicotine-free world. As a nicotine-free world will never exist. There will always be a set % of people who will use nicotine recreationally. The same as there will always be a set percentage of people who use caffeine, or drink alcohol. A Puritan world will never exist. So why not push for more harm reduction methods in all vices that people may have? Thanks again, I always enjoy reading your blogs/ articles.
Firstly, let me say you write very well, you're a pleasure to read. But there is a couple of points I wish to take up. You say:
"Translated into everyday terms, that’s about £0.12 for every cigarette lit—a silent debt paid by the public system and, ultimately, by society as a whole for each puff."
Yes, it is of course true that society pays the costs in healthcare. But isn't this the very reason public healthcare was setup in the first place? Specifically to look after the poor and socially disadvantaged? The very same groups you have pointed out bear most of the harms from smoking? The problem I have with this argument is that it is public health groups, specifically Tobacco Control, who use this argument to lobby for more pain and suffering to be inflicted on these same groups by raising the excise tax on smoking.
You introduce the above by pointing out:
"England alone, smoking accounts for around £2.9 billion annually in healthcare and social care costs."
Ok, but compared to what? How much do Muslims cost in healthcare and social care costs? If I asked this question in public I would be called a racist. It would be pointed out that it is wrong to target a specific group like this. Yet targeting smokers by counting up their costs is perfectly acceptable practice? This in country where public healthcare was deliberately setup to look after the less fortunate?
Furthermore, by what calculation does one come to the conclusion that if all smokers gave up smoking that healthcare and social care costs would diminish? I know you haven't made this argument but it is the implied implication of quoting these costs.
Do non-smoking deaths cost less than smoking deaths? Has anyone ever provided the evidence for this? Would the costs of pensions decrease if everyone gave up smoking? - or would they increase? Would the social care costs be less if all smokers gave up and lived for an extra 5 to 10 years? Who has ever provided any evidence for these implied claims of reducing healthcare and social care costs?
Anyway, I don't mean to be having a go at you personally, I agree with most of what you have written and very much enjoy your writing.